Fentanyl Use Disorder & The Detox Process
Written by: Candice Watts, Clinical Director CADC II
Reviewed by: David Nguyen, MD
Fentanyl, a synthetic opioid up to 100 times more potent than morphine and 50 times more potent than heroin, has become a central figure in the ongoing opioid crisis due to its high risk of dependence, addiction, and fatal overdose1215. As both a prescribed painkiller and an illicit street drug, fentanyl’s potency and rapid onset of action have contributed to a dramatic increase in opioid-related deaths and a surge in individuals struggling with fentanyl use disorder (FUD)117. This article explores the nature of fentanyl use disorder, the symptoms and risks associated with withdrawal, and the best practices for detoxification and recovery.
Understanding Fentanyl Use Disorder
What is Fentanyl?
Fentanyl is a synthetic opioid approved for severe pain management, often in cases of cancer or post-surgical pain. While pharmaceutical fentanyl is administered via patches, lozenges, or injections, illicitly manufactured fentanyl is often found as powders, pills, or mixed with other drugs, greatly increasing overdose risk21517.
How Does Fentanyl Affect the Brain?
Fentanyl binds to opioid receptors in the brain, particularly those involved in pain and emotion regulation. Repeated use leads to tolerance (requiring higher doses for the same effect) and dependence (experiencing withdrawal symptoms when not using)1. Over time, fentanyl use can hijack the brain’s reward system, making it difficult to feel pleasure from anything other than the drug and leading to compulsive drug-seeking behavior-hallmarks of addiction17.
Signs and Symptoms of Fentanyl Use Disorder
Fentanyl use disorder manifests through a combination of behavioral, physical, cognitive, and psychosocial symptoms811:
Behavioral: Continued use despite harm, social withdrawal, neglecting responsibilities, doctor shopping, forging prescriptions.
Physical: Drowsiness, constricted pupils, insomnia, slowed breathing.
Cognitive: Impaired memory and judgment, intense cravings.
Psychosocial: Depression, anxiety, apathy, loss of interest in previously enjoyed activities.
The Dangers of Fentanyl Withdrawal
Why is Fentanyl Withdrawal So Severe?
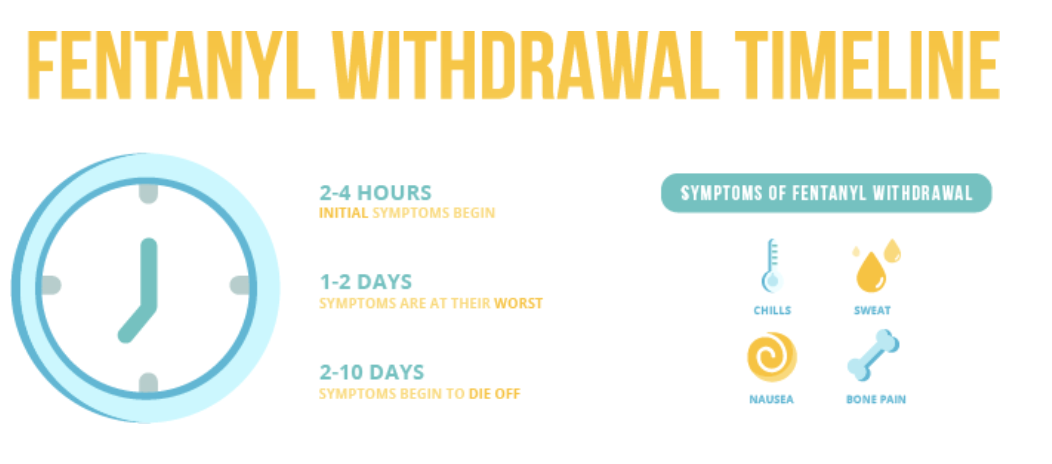
Fentanyl’s high potency and lipophilicity (ability to dissolve in fats) mean it accumulates in the body’s tissues, leading to severe and sometimes prolonged withdrawal symptoms when use stops914. Withdrawal can begin within hours of the last dose and often peaks within a few days, but symptoms may persist for a week or more14. Fentanyl detox symptoms can be intense and challenging, especially due to the drug’s high potency and rapid onset. Individuals who stop using fentanyl often experience withdrawal symptoms within 6 to 12 hours of their last dose. Common fentanyl detox symptoms include severe muscle and bone pain, insomnia, chills, sweating, nausea, vomiting, anxiety, and intense drug cravings. These symptoms typically peak within the first few days but can persist for a week or longer, depending on the individual’s level of dependence and overall health. Because withdrawal can be both physically and emotionally taxing, it's strongly recommended to undergo detox in a medically supervised setting where symptoms can be safely managed and complications minimized.
Common Fentanyl Withdrawal Symptoms
Withdrawal symptoms from fentanyl are similar to those from other opioids but are often more intense and may include1481114:
Muscle and bone pain
Insomnia and sleep disturbances
Nausea, vomiting, diarrhea
Sweating, chills, goosebumps
Anxiety, depression, irritability
Intense cravings for fentanyl
Abdominal cramping
Dilated pupils
Restlessness and agitation
Risks During Fentanyl Withdrawal
The discomfort and severity of withdrawal can lead to dehydration, electrolyte imbalances, and a high risk of relapse. In some cases, withdrawal may be complicated by co-occurring mental health conditions or polysubstance use, further increasing the risk of medical complications314.
The Detox Process: Medical vs. At-Home Approaches
Detoxing from fentanyl is a crucial and often life-saving step for individuals struggling with opioid addiction. This process involves clearing the drug from the body while managing the intense physical and psychological withdrawal symptoms that come with it. Because fentanyl is far more potent than many other opioids, withdrawal can be particularly severe, making it essential to undergo detox under medical supervision. Attempting to go through this alone can be dangerous and overwhelming. Medically supervised programs provide the support and treatment needed to make detoxing from fentanyl as safe and comfortable as possible, increasing the likelihood of a successful transition into long-term recovery.
Why Professional Fentanyl Detox is Recommended
Given the severity of fentanyl withdrawal, medical supervision is strongly recommended341216. A medically supervised detox provides:
24/7 monitoring for complications
Medication management to ease symptoms
Supportive care (hydration, nutrition, emotional support)
Reduced risk of relapse and overdose
Attempting to detox at home, especially after long-term or high-dose fentanyl use, is risky and often unsuccessful due to overwhelming cravings and withdrawal symptoms412.
At-Home Detox: When Is It Appropriate?
In rare cases of mild dependence, at-home detox may be considered if the individual has:
Used fentanyl for a short period at low doses
A stable, supportive, drug-free home environment
No significant medical or psychiatric comorbidities
Strong motivation and support from family/friends
Even in these cases, consultation with a healthcare provider is essential, and plans should be in place for immediate medical help if needed4.
Medications and Strategies for Fentanyl Detox
Medication-Assisted Treatment (MAT)
Medication-Assisted Treatment (MAT) is widely recognized as the gold standard for managing opioid withdrawal and supporting long-term recovery 3451216.. It involves the use of FDA-approved medications that either mimic or block the effects of opioids to ease withdrawal symptoms and reduce cravings.
Always consult a qualified medical provider to determine the safest and most effective treatment plan for you. MAT should only be initiated and monitored under professional medical supervision.
Methadone: A long-acting opioid agonist that reduces withdrawal symptoms and cravings by occupying opioid receptors without producing euphoria516.
Buprenorphine: A partial opioid agonist that eases withdrawal and cravings with a ceiling effect, reducing overdose risk512.
Naltrexone: An opioid antagonist that blocks the effects of opioids but is only used after complete detoxification to prevent relapse45.
Lofexidine and Clonidine: Non-opioid medications that help manage symptoms like anxiety, agitation, and high blood pressure15.
Tapering vs. Cold Turkey
Tapering: Gradually reducing fentanyl dosage, often by switching to a longer-acting opioid like methadone or buprenorphine, is safer and more comfortable than abrupt cessation (“cold turkey”)412. Tapering schedules are individualized based on duration, dose, and other health factors, typically lasting 8–11 days or longer12.
Cold Turkey: Stopping fentanyl suddenly leads to rapid, severe withdrawal and a high risk of relapse. This approach is generally not recommended412.
Symptomatic Support
A range of medications may be used to manage withdrawal symptoms and improve comfort during opiate detox. These may include:
Subutex (buprenorphine) – Helps reduce cravings and withdrawal symptoms
Valium (diazepam) – Used for anxiety, agitation, and muscle spasms
Loperamide – For diarrhea
Promethazine – For nausea and vomiting
Ibuprofen – For muscle aches and general pain
Comprehensive Support
Detox programs also provide:
Hydration and nutrition support
Psychological counseling and emotional support
Preparation for ongoing addiction treatment (rehabilitation, therapy, support groups)312
The Fentanyl Withdrawal Timeline
How long does it take to detox from fentanyl? The answer varies depending on several factors, including the length and severity of use, overall health, and whether medical support is involved. Generally, fentanyl detox can take anywhere from several days to a few weeks. Acute withdrawal symptoms often begin within 6 to 12 hours after the last dose and can peak around days 2 to 4. These symptoms may include muscle pain, anxiety, sweating, insomnia, and intense cravings. However, psychological symptoms and cravings can linger for weeks or even months. Because fentanyl is a potent synthetic opioid, medically supervised detox is strongly recommended to manage symptoms safely and reduce the risk of relapse. If you're wondering how long does it take to detox off fentanyl for yourself or a loved one, seeking help from a professional treatment provider can make the process safer and more effective.
Fentanyl detox centers provide specialized care to help individuals safely navigate the withdrawal process. These centers offer 24/7 medical supervision, emotional support, and often incorporate medication-assisted treatment (MAT) to ease withdrawal symptoms. Choosing a reputable fentanyl detox center can significantly increase the chances of successful recovery by offering a structured and supportive environment. Whether you're just starting your recovery journey or helping someone else, fentanyl detox centers are an essential first step toward long-term sobriety.
Challenges Unique to Fentanyl Detox
Severity and Duration
Emerging research suggests that fentanyl withdrawal is often more severe, longer-lasting, and has a faster onset than withdrawal from heroin or other opioids9. Some individuals may continue to test positive for fentanyl in urine for over a week after cessation, complicating the timing of medication initiation and increasing the risk of precipitated withdrawal (especially with buprenorphine)9.
Relapse Risk
The intense negative emotional states-depression, anxiety, dysphoria-during withdrawal are major drivers of relapse7. Addressing these psychological symptoms is critical for successful detox and long-term recovery.
Polysubstance Use and Contaminants
Illicit fentanyl is often mixed with other drugs (e.g., heroin, cocaine, xylazine), increasing unpredictability of withdrawal and overdose risk1517. This complicates detox and may require additional medical interventions.
After Detox: The Importance of Ongoing Treatment
Detox is only the first step in recovery. While it addresses physical dependence, it does not treat the underlying addiction or the psychological and behavioral aspects of fentanyl use disorder12. Without further treatment, relapse rates are high-up to 80% within the first month post-detox if no ongoing support is provided12.
Inpatient vs. Outpatient Rehabilitation
Inpatient (Residential) Rehab: Provides structured, immersive treatment for those with severe addiction or unstable home environments12
Outpatient Rehab: Allows individuals to receive treatment while maintaining work, school, or family responsibilities1218
Ongoing Therapy and Support
Individual counseling: Addresses personal triggers, trauma, and co-occurring mental health issues12
Family therapy: Improves communication and healing within the family system12
12-step programs (e.g., Cocaine Anonymous): Offers peer support and accountability912
Sober living homes: Provide a drug-free, supportive environment during early recovery12
Relapse Prevention
Relapse is common in addiction recovery but does not signify failure9. Effective relapse prevention includes:
Identifying triggers: Stress, social situations, or emotional distress912
Developing coping skills: Stress management, mindfulness, and healthy hobbies12
Building a support network: Friends, family, therapists, and peer groups912
Regular follow-up: Ongoing check-ins with healthcare providers12
Seeking Help: When and How
If you or someone you know is struggling with fentanyl use, seek help as soon as possible. Warning signs that professional intervention is needed include:
Inability to stop using despite repeated attempts9
Neglect of personal, work, or family responsibilities9
What to Do:
Contact a healthcare provider: Addiction specialists or mental health professionals can assess the situation and recommend treatment84.
Call a helpline: National helplines provide free, confidential support and referrals.
Reach out to local resources: Community health centers, hospitals, and nonprofit organizations often provide addiction treatment services.
Conclusion
Fentanyl use disorder is a life-threatening condition requiring comprehensive, compassionate care. The detox process is challenging, with severe withdrawal symptoms and a high risk of relapse. Medically supervised detox, supported by medication-assisted treatment and holistic care, offers the safest and most effective path to recovery. However, detox is only the beginning-ongoing treatment and support are essential for long-term success.
If you or a loved one is seeking compassionate, professional support on the journey to recovery, Solace Health offers personalized addiction services—from detox coordination to sober coaching—tailored to meet your unique needs. Let our experienced team help guide you toward lasting healing and freedom.
Solace Health Group conducts thorough research, includes trusted citations, and ensures all content is reviewed for accuracy. However, this article is not medical advice and should not replace professional evaluation or treatment. Always consult a licensed healthcare provider before making any medical or treatment decisions.
Sources:
Opioid Use Disorder - StatPearls - NCBI Bookshelf
https://www.ncbi.nlm.nih.gov/books/NBK553166/
Opioid Use Disorder - Psychiatry.org
https://www.psychiatry.org/patients-families/opioid-use-disorder
CDC Reports Nearly 24% Decline in U.S. Drug Overdose Deaths
https://www.cdc.gov/media/releases/2025/2025-cdc-reports-decline-in-us-drug-overdose-deaths.html
Co-occurring illicit fentanyl use and psychiatric disorders in emergency department patients
https://www.nature.com/articles/s41598-025-92311-2
The rising crisis of illicit fentanyl use, overdose, and potential clinical management
https://www.nature.com/articles/s41398-019-0625-0
Medications for Opioid Use Disorder | National Institute on Drug Abuse (NIDA)
https://nida.nih.gov
Opioid Use and Opioid Use Disorder in Pregnancy - ACOG
https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2017/08/opioid-use-and-opioid-use-disorder-in-pregnancy
Examining the association between fentanyl use and perceived methadone effectiveness
https://www.sciencedirect.com/science/article/abs/pii/S0376871624014728
How opioid use disorder occurs - Mayo Clinic
https://www.mayoclinic.org/diseases-conditions/prescription-drug-abuse/in-depth/how-opioid-addiction-occurs/art-20360372
Understanding the Opioid Overdose Epidemic - CDC
https://www.cdc.gov/overdose-prevention/about/understanding-the-opioid-overdose-epidemic.html